The Peri-Medi Diet: What To Eat During Perimenopause
10 Ways to Modify the Mediterranean Diet During Perimenopause
Hello, everyone.
I am writing to you from Ortigia, Sicily as we wrap up another Brain Health Retreat. Since I have a few days off until my next retreat starts in Palermo, I am going to drive my little Fiat a few hours north of the city to visit the place where my grandparents were born. My father’s mom and dad grew up on the same street in Santa Caterina, a tiny town perched high in the mountains of central Sicily. While my grandparents left impoverished, post-war Sicily in the to find a better life in Rochester, NY, many of my relatives remained. I am excited to meet all my distant cousins and explore this part of Italy that has been studied for the longevity of its people.
Would you like to hear more about my experiences visiting relatives in Sicily? Let me know and I’ll report back in a dedicated post.
Today we are talking about what to eat during perimenopause—the years leading up to and just after menopause.
Let’s get this out of the way up front: I am not going to tell you to load up on flaxseeds or tofu or pomegranate seeds as some sort of magic bullet to get rid of your hot flashes and night sweats. This “superfood” approach has failed miserably in scientific studies. It’s not as simple as just “eat this and not that.” The good news is that just like eating to reduce the risk of dementia, there is a growing body of science that supports a pattern of eating that may alleviate perimenopausal symptoms.
Plus, eating this way can check off other important health goals for women during perimenopause. It can:
Prevent loss of bone density
Build and maintain muscle mass
Keep blood sugar stable
Push back against changes in body weight and composition
Identify and reverse risk factors for heart disease and dementia
So for today’s newsletter, let’s look at the Mediterranean dietary pattern from the point of view of a perimenopausal woman. I’m calling it the Peri-Medi Dietary Pattern, and I outline what this means below.
Perimenopause and me, we go way back
I may be dating myself here, but back in 1990 I gave a grand rounds presentation about perimenopause to the ob/gyn physicians where I trained. The word “perimenopause” was new then and this was the first time many had heard of it. I went on to become a card-carrying member of the North American Menopause Society and took a board exam to become one of a handful of menopause specialists in the country. During the years when I specialized in menopause, circa 2000 to 2010, I held free educational town hall-style talks I called “Menopause Workshops.” Everyone was welcome to come and ask questions like how to prevent osteoporosis or the pros and cons of HRT. When the 2002 Women’s Health Initiative released their now-famously flawed statement that estrogen causes breast cancer, I held an emergency Menopause Workshop and I think every woman in town was there.
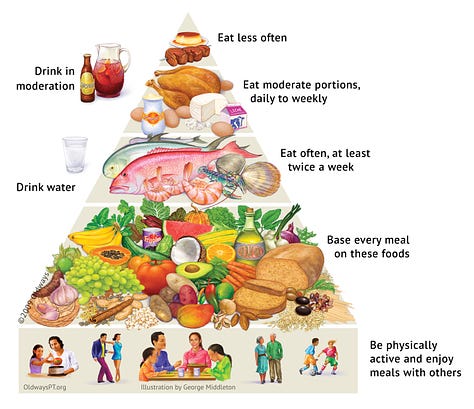
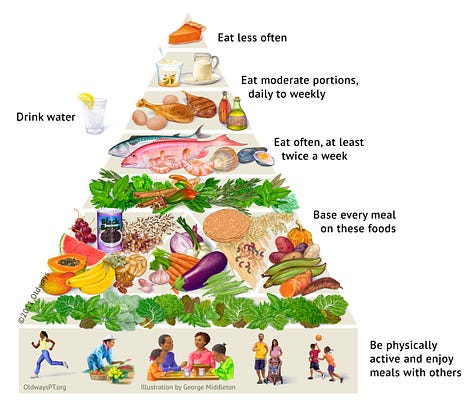
All of this is to say that I am writing to you as someone who cares deeply about women at this stage of life. And, for what it’s worth, my personal experience of taking care of thousands of patients mirrors the latest research: women who follow a Mediterranean-style diet tend to weather the perimenopause better, with fewer and less severe symptoms. Even though no one was really talking about nutrition during menopause back then, I’m glad I kept a stack of Mediterranean diet pyramid handouts—in full color—in my desk drawer to give to every perimenopausal patient I saw.
Mediterranean diet and perimenopause
When it comes to brain health, there are over 100 high-quality studies that support following a Mediterranean-style diet, or one of its spin-offs, such as the MIND and Green MED patterns. For perimenopause, there isn’t the same volume of data. What we do have is this: a handful of promising studies that show that when Mediterranean dietary guidelines are closely followed, women experience fewer and less severe perimenopausal symptoms. The evidence here is stronger than with any other eating pattern.

In a nutshell, the Mediterranean diet emphasizes these food groups: vegetables, beans and legumes, fruit, whole grains, fish and seafood, nuts and seeds, olive oil. It includes fewer servings of dairy products, meat, chicken, and eggs. Sweets are eaten sparingly and processed foods are avoided. Red wine is included in small portions with some meals, which are shared with family and friends all in the context of an active lifestyle.
This Medi diet study of over 6,000 women singled out vasomotor symptoms like hot flashes and night sweats. The more closely women followed a Medi diet, the less of these symptoms they experienced. In this Italian study of overweight women, those who adhered closely to the Medi guidelines reported fewer symptoms overall, especially if beans and legumes were consumed at target levels (4 servings a week, each about ½ cup, cooked). They also found that psychological symptoms (like mood instability) were reduced as the amount of olive oil in the diet went up.
Other studies have looked at how key components of the Mediterranean diet may reduce perimenopausal symptoms, with mixed results. There is evidence that limiting or avoiding processed food is beneficial, as is improving carbohydrate quality (such as swapping in whole grains for refined ones). Researchers haven’t been able to prove, however, that boosting isoflavones (flavonoids with weak estrogen effects) nor omega-3s, either with food or supplements, is effective. And this low fat, plant-based dietary intervention looked promising, but it was only followed for 12 weeks, not enough time to get past the placebo effect.

You may already be following the Mediterranean diet. To see how you’re doing, take my fun quiz: How Mediterranean Is Your Diet?
Taking stock of your health during perimenopause
As I used to say in my menopause workshops all those years ago: Perimenopause is an opportunity. It’s a chance to take stock of your current health. It’s a time to evaluate what’s working, or not, and plan for a healthy future. This hinges on gathering some information about your current health. The goal: enter perimenopause informed and with a plan. Here’s a checklist to get you started.
Bone density test. Knowing your baseline bone density serves to flag any problems, while helping inform the decision to take menopausal hormone therapy later. Read Bone Health 101 here.
Blood cholesterol. A full lipid panel including LDL, ApoB, and Lp (a) will help you know where you stand with these heart- and brain health biomarkers. Read Cholesterol 101 here and don’t miss the helpful glossary of terms here.
Body weight. Notice if weight is trending up or down, and measure a hip-to-waist ratio for baseline. I walk you through how to do this here.
Blood pressure. Midlife is the time to aggressively get blood pressure under target levels: less than 120 over 80. More here.
Blood sugar. Fasting blood sugar and hemoglobin A1c can creep up during perimenopause and signal a tendency to insulin resistance, type 2 diabetes, or metabolic syndrome. Read more about how perimenopause impacts metabolic health here.
ApoE4. Carrying one or two copies of this gene variant may impact how a woman’s brain weathers the perimenopause. Knowing one’s carrier status may help with decisions to take HRT; this study found HRT to be especially protective if taken early in the transition period. Learn more here about the pros and cons of getting tested.
In addition, perimenopause is a good time to double check to see if you have a family history of cancer, heart disease, Alzheimer’s, or other dementias. If possible, reflect on other aspects of your life. How’s your mental health? How are you sleeping? Do you have a plan to mitigate stress?
I know it’s a lot, but all of these things become an integral part of your perimenopause experience.
The Peri-Medi Diet: 10 Ways to Modify the Medi Diet for Perimenopause






